Physiological Correlates of HRV Components
Physiological Correlates of HRV Components
Autonomic Influences of Heart Rate
Although cardiac automaticity is intrinsic to various pacemaker tissues, heart rate and rhythm are largely under the control of the autonomic nervous system. The parasympathetic influence on heart rate is mediated via release of acetylcholine by the vagus nerve. Muscarinic acetylcholine receptors respond to this release mostly by an increase in cell membrane K+ conductance. Acetylcholine also inhibits the hyperpolarization-activated “pacemaker” current If.
The “Ik decay” hypothesis proposes that pacemaker depolarization results from slow deactivation of the delayed rectifier current, Ik, which, due to a time-independent background inward current, causes diastolic depolarization.
Conversely, the “If activation” hypothesis suggests that after action potential termination, If provides a slowly activating inward current predominating over decaying Ik, thus initiating slow diastolic depolarization.
The sympathetic influence on heart rate is mediated by release of epinephrine and norepinephrine. Activation of ßadrenergic receptors results in cAMP-mediated phosphorylation of membrane proteins and increases in ICaL and in If. The end result is an acceleration of the slow diastolic depolarization.
Under resting conditions, vagal tone prevails and variations in heart period are largely dependent on vagal modulation. The vagal and sympathetic activity constantly interacts. Because the sinus node is rich in acetylcholinesterase, the effect of any vagal impulse is brief because the acetylcholine is rapidly hydrolyzed.
Parasympathetic influences exceed sympathetic effects probably through two independent mechanisms: (1) a cholinergically induced reduction of norepinephrine released in response to sympathetic activity and (2) a cholinergic attenuation of the response to an adrenergic stimulus.
Components of HRV
Although HRV has been the subject of numerous clinical studies investigating a wide spectrum of cardiological and noncardiological diseases and clinical conditions, a general consensus of the practical use of HRV in adult medicine has been reached only in two clinical scenarios. Depressed HRV can be used as a predictor of risk after acute MI and as an early warning sign of diabetic neuropathy.
The RR interval variations present during resting conditions represent a fine tuning of the beat-to-beat control mechanisms. Vagal afferent stimulation leads to reflex excitation of vagal efferent activity and inhibition of sympathetic efferent activity. The opposite reflex effects are mediated by the stimulation of sympathetic afferent activity. Efferent vagal activity also appears to be under “tonic” restraint by cardiac afferent sympathetic activity.
Efferent sympathetic and vagal activities directed to the sinus node are characterized by discharge largely synchronous with each cardiac cycle that can be modulated by central (vasomotor and respiratory centers) and peripheral (oscillation in arterial pressure and respiratory movements) oscillators. These oscillators generate rhythmic fluctuations in efferent neural discharge that manifest as short- and long-term oscillation in the heart period. Analysis of these rhythms may permit inferences on the state and function of (a) the central oscillators, (b) the sympathetic and vagal efferent activity, (c) humoral factors, and (d) the sinus node.
An understanding of the modulatory effects of neural mechanisms on the sinus node has been enhanced by spectral analysis of HRV. The efferent vagal activity is a major contributor to the HF component, as seen in clinical and experimental observations of autonomic maneuvers such as electrical vagal stimulation, muscarinic receptor blockade, and vagotomy. More controversial is the interpretation of the LF component, which is considered by some as a marker of sympathetic modulation (especially when expressed in normalized units) and by others as a parameter that includes both sympathetic and vagal influences. This discrepancy is due to the fact that in some conditions associated with sympathetic excitation, a decrease in the absolute power of the LF component is observed. It is important to recall that during sympathetic activation the resulting tachycardia is usually accompanied by a marked reduction in total power, whereas the reverse occurs during vagal activation. When the spectral components are expressed in absolute units (milliseconds squared), the changes in total power influence LF and HF in the same direction and prevent the appreciation of the fractional distribution of the energy. This explains why in supine subjects under controlled respiration, atropine reduces both LF and HF and why during exercise LF is markedly reduced.However, after normalization an increase in LF becomes evident. Similar results apply to the LF/HF ratio.
Spectral analysis of 24-hour recordings shows that in normal subjects, LF and HF expressed in normalized units exhibit a circadian pattern and reciprocal fluctuations, with higher values of LF in the daytime and of HF at night. These patterns become undetectable when a single spectrum of the entire 24-hour period is used or when spectra of subsequent shorter segments are averaged. In long-term recordings, the HF and LF components account for only approximately 5% of total power. Although the ULF and VLF components account for the remaining 95% of total power, their physiological correlates are still unknown.
LF and HF can increase under different conditions. An increased LF (expressed in normalized units) is observed during 90° tilt, standing, mental stress, and moderate exercise in healthy subjects, and during moderate hypotension, physical activity, and occlusion of a coronary artery or common carotid arteries in conscious dogs. Conversely, an increase in HF is induced by controlled respiration, cold stimulation of the face, and rotational stimuli.
Summary and Recommendations for Interpretation of HRV Components. Vagal activity is the major contributor to the HF component.
Disagreement exists in respect to the LF component. Some studies suggest that LF, when expressed in normalized units, is a quantitative marker of sympathetic modulations; other studies view LF as reflecting both sympathetic activity and vagal activity. Consequently, the LF/HF ratio is considered by some investigators to mirror sympathovagal balance or to reflect the sympathetic modulations.
Physiological interpretation of lower-frequency components of HRV (that is, of the VLF and ULF components) warrants further elucidation.
It is important to note that HRV measures fluctuations in autonomic inputs to the heart rather than the mean level of autonomic inputs. Thus, both autonomic withdrawal and saturating high level of sympathetic input lead to diminished HRV.
Changes of HRV Related to Specific Pathologies.
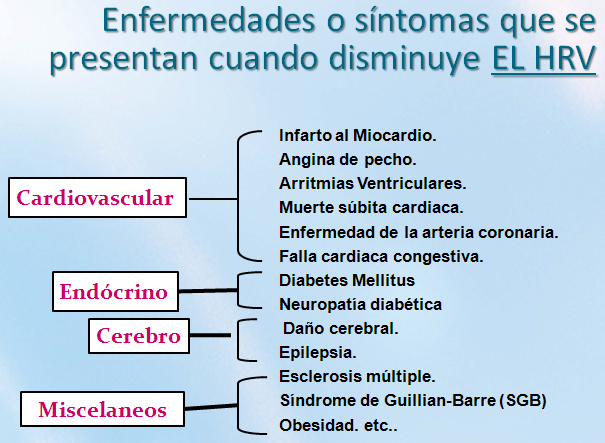
A reduction of HRV has been reported in several cardiological and noncardiological diseases.
Myocardial Infarction
Depressed HRV after MI may reflect a decrease in vagal activity directed to the heart, which leads to prevalence of sympathetic mechanisms and to cardiac electrical instability. In the acute phase of MI, the reduction in 24-hour SDNN is significantly related to left ventricular dysfunction, peak creatine kinase, and Killip class. The mechanism by which HRV is transiently reduced after MI and by which a depressed HRV is predictive of the neural response to acute MI is not yet defined, but it is likely to involve derangements in the neural activity of cardiac origin.
One hypothesis involves cardiocardiac sympathosympathetic and sympathovagal reflexes and suggests that the changes in the geometry of a beating heart due to necrotic and noncontracting segments may abnormally increase the firing of sympathetic afferent fibers by mechanical distortion of the sensory endings. This sympathetic excitation attenuates the activity of vagal fibers directed to the sinus node. Another explanation, especially applicable to marked reduction of HRV, is the reduced responsiveness of sinus nodal cells to neural modulations.
Spectral analysis of HRV in patients surviving an acute MI revealed a reduction in total and in the individual power of spectral components. However, when the power of LF and HF was calculated in normalized units, an increased LF and a diminished HF were observed during both resting controlled conditions and 24-hour recordings analyzed over multiple 5-minute periods. These changes may indicate a shift of sympathovagal balance toward a sympathetic predominance and a reduced vagal tone. Similar conclusions were obtained by considering the changes in LF/HF ratio. The presence of an alteration in neural control mechanisms was also reflected by the blunting of the day-night variations of RR interval and LF and HF spectral components present in a period ranging from days to a few weeks after the acute event. In post-MI patients with a very depressed HRV, most of the residual energy is distributed in the VLF frequency range below 0.03 Hz, with only a small respiration-related HF. These characteristics of the spectral profile are similar to those observed in an advanced cardiac failure or after cardiac transplant and are likely to reflect either a diminished responsiveness of the target organ to neural modulatory inputs or a saturating influence on the sinus node of a persistently high sympathetic tone.
Diabetic Neuropathy
In neuropathy associated with diabetes mellitus characterized by alteration of small nerve fibers, a reduction in time domain parameters of HRV seems not only to carry negative prognostic value but also to precede the clinical expression of autonomic neuropathy. In diabetic patients without evidence of autonomic neuropathy, reduction of the absolute power of LF and HF during controlled conditions was also reported. However, when the LF/HF ratio was considered or when LF and HF were analyzed in normalized units, no significant difference in comparison to normal subjects was present. Thus, the initial manifestation of this neuropathy is likely to involve both efferent limbs of the autonomic nervous system.
Cardiac Transplantation
A very reduced HRV with no definite spectral components was reported in patients with a recent heart transplant. The appearance of discrete spectral components in a few patients is considered to reflect cardiac reinnervation. This reinnervation may occur as early as 1 to 2 years after transplantation and is usually of sympathetic origin. Indeed, the correlation between the respiratory rate and the HF component of HRV observed in some transplanted patients also indicates that a nonneural mechanism may contribute to generate a respiration-related rhythmic oscillation. The initial observation of identifying patients developing an allograft rejection according to changes in HRV could be of clinical interest but needs further confirmation.
Myocardial Dysfunction
A reduced HRV has been observed consistently in patients with cardiac failure. In this condition characterized by signs of sympathetic activation such as faster heart rates and high levels of circulating catecholamines, a relation between changes in HRV and the extent of left ventricular dysfunction was reported. In fact, whereas the reduction in time domain measures of HRV seemed to parallel the severity of the disease, the relationship between spectral components and indices of ventricular dysfunction appears to be more complex. In particular, in most patients with a very advanced phase of the disease and with a drastic reduction in HRV, an LF component could not be detected despite the clinical signs of sympathetic activation. Thus, in conditions characterized by a marked and unopposed persistent sympathetic excitation, the sinus node seems to drastically diminish its responsiveness to neural inputs.
Tetraplegia
Patients with chronic complete high cervical spinal cord lesions have intact efferent vagal and sympathetic neural pathways directed to the sinus node. However, spinal sympathetic neurons are deprived of modulatory control and in particular of baroreflex supraspinal inhibitory inputs. For this reason, these patients represent a unique clinical model to evaluate the contribution of supraspinal mechanisms in determining the sympathetic activity responsible for LF oscillations of HRV. It has been reported that no LF could be detected in tetraplegic patients, thus suggesting the critical role of supraspinal mechanisms in determining the 0.1 Hz rhythm. Two recent studies, however, have indicated that an LF component also can be detected in HRV and arterial pressure variabilities of some tetraplegic patients. While Koh et al attributed the LF component of HRV to vagal modulations, Guzzetti et al attributed the same component to sympathetic activity because of the delay with which the LF component appeared after spinal section, suggesting an emerging spinal rhythmicity capable of modulating sympathetic discharge.
Modifications of HRV by Specific Interventions
The rationale for trying to modify HRV after MI stems from the multiple observations indicating that cardiac mortality is higher among those post-MI patients who have a more depressed HRV. The inference is that interventions that augment HRV may be protective against cardiac mortality and sudden cardiac death. Although the rationale for changing HRV is sound, it also contains the inherent danger of leading to the unwarranted assumption that modification of HRV translates directly into cardiac protection, which may not be the case. The target is the improvement of cardiac electrical stability, and HRV is just a marker of autonomic activity. Despite the growing consensus that increases in vagal activity can be beneficial, it is not as yet known how much vagal activity (or its markers) has to increase in order to provide adequate protection.
ß-Adrenergic Blockade and HRV
The data on the effect of ß-blockers on HRV in post-MI patients are surprisingly scant. Despite the observation of statistically significant increases, the actual changes are very modest. However, it is of note that ß-blockade prevents the rise in the LF component observed in the morning hours. In conscious post-MI dogs, ß-blockers do not modify HRV. The unexpected observation that before MI, ß-blockade increases HRV only in the animals destined to be at low risk for lethal arrhythmias after MI may suggest novel approaches to post-MI risk stratification.
Antiarrhythmic Drugs and HRV
Data exist for several antiarrhythmic drugs. Flecainide and propafenone but not amiodarone were reported to decrease time domain measures of HRV in patients with chronic ventricular arrhythmia. In another study, propafenone reduced HRV and decreased LF much more than HF, resulting in a significantly smaller LF/HF ratio. A larger study confirmed that flecainide, also encainide and moricizine, decreased HRV in post-MI patients but found no correlation between the change in HRV and mortality during follow-up. Thus, some antiarrhythmic drugs associated with increased mortality can reduce HRV. However, it is not known whether these changes in HRV have any direct prognostic significance.
Scopolamine and HRV
Low-dose muscarinic receptor blockers, such as atropine and scopolamine, may produce a paradoxical increase in vagal efferent activity, as suggested by a decrease in heart rate. Different studies examined the effects of transdermal scopolamine on indices of vagal activity in patients with a recent MI and with congestive heart failure. Scopolamine markedly increases HRV, which indicates that pharmacological modulation of neural activity with scopolamine may effectively increase vagal activity. However, the efficacy during long-term treatment has not been assessed. Furthermore, low-dose scopolamine does not prevent ventricular fibrillation caused by acute myocardial ischemia in post-MI dogs.
Thrombolysis and HRV
The effect of thrombolysis on HRV (assessed by pNN50) was reported in 95 patients with acute MI. HRV was higher 90 minutes after thrombolysis in the patients with patency of the infarct-related artery. However, this difference was no longer evident when the entire 24 hours were analyzed.
Exercise Training and HRV
Exercise training may decrease cardiovascular mortality and sudden cardiac death. Regular exercise training is also thought capable of modifying the autonomic balance. A recent experimental study designed to assess the effects of exercise training on markers of vagal activity has simultaneously provided information on changes in cardiac electrical stability. Conscious dogs documented to be at high risk by the previous occurrence of ventricular fibrillation during acute myocardial ischemia were randomly assigned to 6 weeks of either daily exercise training or cage rest followed by exercise training. After training, HRV (SDNN) increased by 74%, and all animals survived a new ischemic test. Exercise training can also accelerate recovery of the physiological sympathovagal interaction, as shown in post-MI patients.